One of the hardest parts of seeing a soldier return home from combat is seeing the heavy price they paid in service to our country. At first glance, it’s easy to notice someone missing a limb, but it’s almost impossible to look at someone and see the traumatic brain injuries they may have suffered during their service. As a result, there’s a bit of a disconnect among the general population and their understanding of just how devastating a traumatic brain injury can be for our servicemen and women.
The Link Between TBI and Veterans
In 2020, traumatic brain injuries (TBIs for short) were responsible for over 64,000 deaths in the U.S. alone. While not all of these were military veterans, you can find an especially strong link between military service and traumatic brain injuries by looking at a bit of additional data for context.
For example, did you know that the leading cause of traumatic brain injuries is firearm assisted suicide? Or that around 72% of veteran suicides are from firearms, 22% higher than the national average? Considering that U.S. veterans are a little over twice as likely to own a gun than the average citizen, it becomes all too easy to connect the dots and see that veterans are especially at risk of TBI’s even long after they’ve returned home.
Aside from the suicide risk, the vast majority of veterans receive their TBI’s in combat. Soldiers in the field can be surrounded day and night by explosions, bullets, and even falling debris, any of which can cause a TBI. In fact, such injuries are actually the leading cause of both death and disabilities in warzones. U.S. House of Representatives member, Bill Pascrell, even went so far as to call TBI “the signature injury of the wars in Iraq and Afghanistan”, further driving home the fact that traumatic brain injuries are more common among veterans than most people realize.
It’s easy to think that somebody returning home from service appears to be physically healthy and without scars from their time away. But the brain is by far the most important and delicate organ in our entire body, which is why internal brain injuries like TBIs can be so devastating to someone who may otherwise appear perfectly fine on the outside.
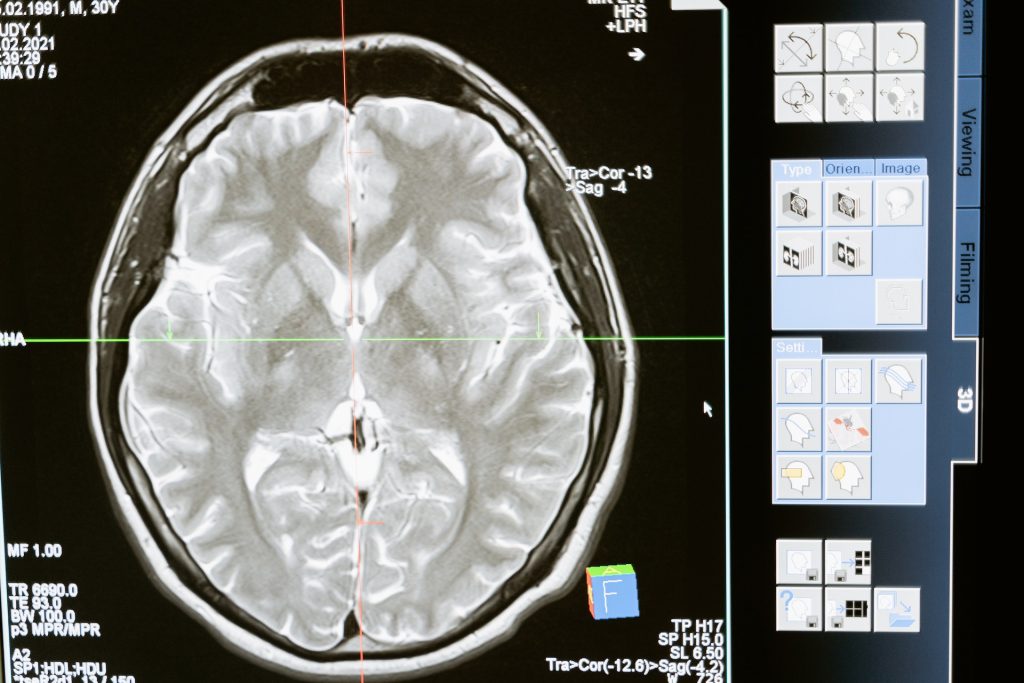
Diagnosing a Traumatic Brain Injury
In order to understand how to diagnose a TBI, it’s important to know a little more about how they cause their damage.
The first thing to know is that not all of the injury takes place at once. A “primary brain injury” occurs at the actual time of the injury, while a “secondary brain injury” may slowly manifest and cause additional damage over time. In essence, just because a brain injury might not be immediately devastating, it does not mean that it can’t eventually be devastating if left untreated.
This is why seeking a medical professional as soon as possible after the primary brain injury is so important. While any official TBI diagnosis should come from a qualified doctor, there are a few things that can tip you off to a potential sustained TBI that could save you valuable days, weeks, or months worth of additional secondary brain damage.
The first and most obvious question to answer is a simple one: Did you sustain any kind of head-related injury? Even something as simple as bumping your head on the ceiling of an attic can lead to a TBI, so don’t hesitate to see a doctor if you’re suffering from non-typical headaches or especially any periods of unconsciousness right in the aftermath of the injury.
You should also be on the lookout for “vomiting, nausea, lack of motor coordination, dizziness, difficulty balancing, lightheadedness, blurred vision or tired eyes, ringing in the ears, bad taste in the mouth, fatigue or lethargy, and changes in sleep patterns,” according to the National Institute of Neurological Disorders and Stroke. An especially obvious sign can be pupils of two different dilation levels.
Unfortunately, not all the symptoms of a TBI are so easy to spot. Sometimes a TBI can take much longer to manifest thanks to additional secondary brain damage, which can lead to gradual changes in personality or even decision-making capabilities over a long period time. Thankfully, these more subtle symptoms often come in tandem with at least a few of the more obvious physical symptoms, so if you or someone you know has been suffering from symptoms of both types then it’s time to see a doctor.
Are you a veteran in need of assistance? Click this link for a list of resources made specifically for you. If you’re having suicidal thoughts, please call either The National Veterans’ Foundation at 1-888-777-4443 or the VA Suicide Prevention Hotline at 1-800-273-TALK (800-273-8255). Both hotlines are free and confidential.
If you’re not a veteran but would still like to help out, you can get involved through our donation page here.